Sickle Cell Definition
Sickle cell is an inherited blood disorder in which the red blood cells (RBCs) that carry oxygen around the body develops abnormally.
In sickle cell anemia the shape of the cell becomes deformed, they become rigid and shaped like a crescent (or sickle). The sickle-shaped red blood cells break apart easily, causing anemia .Sickle blood cells cannot function properly & undergo premature death (they live only 10-20 days instead of the normal 120 days).
Get in Touch with Medical Experts
The sickle-shaped cells contain defective hemoglobin. People with sickle cell conditions make a different form of hemoglobin A called hemoglobin S (S stands for sickle These abnormal cells are unable to move around as easily as normal shaped cells and can block blood vessels, resulting in tissue and organ damage and episodes of severe pain. (These cells clump together and stick to the walls of blood vessels, blocking blood flow.)
These episodic pains are known as a sickle cell crisis or a vaso-occlusive crisis. A person may not know what brought on the pain, but infection and dehydration are common triggers. They can last from a few minutes to several months, although on average most last five to seven days.
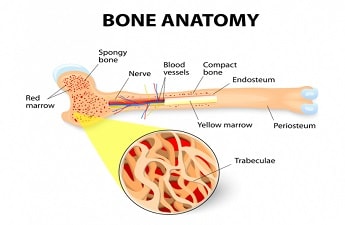
Red blood cells contain hemoglobin, a protein that carries oxygen in the blood. Normal red blood cells are soft , round and flexible (can squeeze through tiny blood vessels), which enables them to travel through small blood vessels to deliver oxygen to all parts of the body Normally, red blood cells live for about 120 days before new ones replace them.
Hemoglobin is the main substance of the red blood cell. It helps RBC’s carry oxygen from the air in our lungs to all parts of the body. Normal red blood cells contain hemoglobin A. Hemoglobin S and hemoglobin C are abnormal types of hemoglobin.
Know More:
Sickle Cell Anemia Causes
Sickle Cell Anemia Genetics
Sickle cell is caused by genetic mutation (an abnormal) change in the gene that affects the normal development of hemoglobin.
A genetic mutation is a permanent change in the normal pattern of genetic information inside all living cells. This results in one or more of the body's processes not working properly.
The sickle cell gene is inherited autosomal recessive pattern (passed on between family members). To get sickle cell anemia you have to inherit the defective gene from both parents. This means that a child will not inherit the disease unless both parents pass down a defective copy of the gene. People who inherit one good copy of the gene and one mutated copy are carriers. They are clinically normal, but can still pass the defective gene to their children.
The chances of sickle cell anemia being passed on are:
-
a one in four chance that your baby will receive a pair of normal hemoglobin genes
-
a one in two chance that your baby will receive one normal gene and one mutated gene and be a carrier of the sickle cell gene
-
a one in four chance that your baby will receive a pair of mutated genes and have sickle cell anemia
What is Sickle Cell Anemia Trait?
People who inherit one sickle cell gene and one normal gene have sickle cell trait (SCT). Sickle cell trait is not regarded as a disease state because it has complications that are either uncommon or mild.
It's likely that there blood will contain some sickle cells, but they will be able to produce normal hemoglobin and won't usually experience symptoms. However, they will be a carrier of sickle cell anemia and may pass the abnormal gene on to their children
How Sickle Cell Trait is inherited:
-
If both parents have SCT, there is a 50% (or 1 in 2) chance that any child of theirs also will have SCT, if the child inherits the sickle cell gene from one of the parents. Such children will not have symptoms of SCD, but they can pass SCT on to their children.
-
If both parents have SCT, there is a 25% (or 1 in 4) chance that any child of theirs will have SCD. There is the same 25% (or 1 in 4) chance that the child will not have SCD or SCT.
Diagnosis:
SCT is diagnosed with a simple blood test. People at risk of having SCT can talk with a doctor or health clinic about getting this test.
A normal blood examination is done which includes:
-
normal red cell morphology,
-
indices,
-
reticulocyte counts,
-
Red blood cell survival by chromium labeling.
Sickle Cell Anemia Symptoms
Sickle cell disease prevents oxygen from reaching the spleen, liver, kidneys, lungs, heart, or other organs, causing a lot of damage. Without oxygen, the cells that make up these organs die.
Sickle cell can cause a wide range of symptoms, although not everyone with the condition will experience all of the symptoms. Some features of sickle cell anemia, such as fatigue, anemia, pain crises, and bone infarcts can occur at any age. Many features typically occur in certain age groups.
Signs and symptoms of sickle cell anemia often don't appear until an infant is at least 4 months old and may include:
Anemia
Sickle cell causes a chronic form of anemia which can lead to fatigue. The sickled red blood cells are prone to breakage (hemolysis) which causes reduced red blood cell life span (the normal life span of a red blood cell is 120 days). This results in a lasting shortage of red blood cells (anemia).
Without enough red blood cells in circulation, body can't get the oxygen it needs to feel energized. That's why anemia causes fatigue.
Symptoms of anemia include:
-
fatigue – extreme tiredness and a general lack of energy
-
shortness of breath
-
palpitations (irregular heartbeat)
Episodes of pain
Periodic episodes of pain, called crises, are a major symptom of sickle cell. Pain crises in persons with sickle cell anemia are intermittent painful episodes that are the result of inadequate blood supply to body tissues. The impaired circulation is caused by the blockage of various blood vessels from the sickling of red blood cells.
The sickled red blood cells slow or completely impede the normal flow of blood through the tissues. This leads to excruciating pain, often requiring hospitalization and medication for relief.
The pain typically is throbbing and can change its location from one body area to another. Bones are frequently affected. Pain in the abdomen with tenderness is common and can mimic appendicitis. Fever frequently is associated with the pain crises.
A person may not know what brought on the pain, but one or more of the following situations may trigger the painful sickle crisis:
-
Dehydration
-
Infection
-
Fever
-
Hypoxia
-
Bleeding
-
Cold exposure
-
Drug & alcohol use
-
Pregnancy & stress
Bacterial Infection
Lung infection (pneumonia) is extremely common in children with sickle cell anemia and is also the most common reason for hospitalization.
Children with sickle cell anemia are also at risk for infection of the brain and spinal fluid (meningitis). Bacteria that are frequent causes of this infection include the Pneumococcus and Haemophilus bacteria
Dactylitis and Arthritis
Swelling and inflammation of the hands and/or feet is often an early sign of sickle cell anemia. The swelling involves entire fingers and/or toes and is called Dactylitis
Swollen hands and feet may be the first signs of sickle cell anemia in babies. The swelling is caused by sickle-shaped red blood cells blocking blood flow out of their hands and feet.
Joint inflammation (arthritis) with pain, swelling, tenderness, and limited range of motion can accompany the dactylitis. Sometimes, not only the joints of the hands or feet are affected, but also a knee or an elbow.
Splenic Sequestration and Liver Congestion
Liver and spleen, are organs that are very active in removing sickled red blood cells from the circulation of persons with sickle cell anemia. This process can accelerate suddenly. Sudden pooling of blood in the spleen is referred to as splenic sequestration. These patients can develop shock and lose consciousness. Splenic sequestration can cause very severe anemia and even result in death.
Lung and Heart Injury
Aside from lung infection (pneumonia), the lungs of children with sickle cell anemia can also be injured by inadequate circulation of blood which causes areas of tissue death. This lung damage can be difficult to distinguish from pneumonia and is known as acute chest syndrome. These localized areas of lung tissue damage are referred to as pulmonary infarcts
The heart is frequently enlarged in children with sickle cell anemia. Rapid heart rates and murmurs are common. The heart muscle can also be injured by infarcts and iron depositing in the muscle as it leaks from the ruptured red blood cells. Over the time, the heart muscle weakens and the heart pumps blood more and more poorly.
Leg ulcers
The legs of patients with sickle cell anemia are susceptible to skin breakdown and ulceration. Leg ulcers most commonly occur in adults and usually form over the ankles and sides of the lower legs. The ulcers can become severe, even encircling the leg, and are prone to infection.
Aseptic Necrosis and Bone Infarcts
Aseptic necrosis, or localized bone death, is a result of inadequate oxygen supply to the bone. It is also referred to as osteonecrosis. While virtually any bone can be affected, the most common are the bones of the thighs, legs, and arms. The result can permanently damage or deform the hips, shoulders, or knees.
Signs of aseptic necrosis includes:
-
Pain
-
Tenderness
-
Disability
Eye Damage
Some people with sickle cell anemia experience vision problems. Tiny blood vessels that supply the eyes may become plugged with sickle cells. This can damage the retina — the portion of the eye that processes visual images. Bleeding can also occur within the eye (retinal hemorrhage) and retinal detachment can result. Retinal detachment can lead to blindness
Additional Symptoms:
-
Osteoporosis causing weakening of bones
-
Kidney damage & infection
-
Nervous system damage: poor circulation in the brain can cause stroke, convulsions & come.
-
Priapism: an abnormally persistent erection of the penis in the absence of sexual desire, can occur in persons with sickle cell anemia. Priapism can lead to impotence and damage to affected tissues
Test & Diagnosis
Sickle cell tests are used to identify the presence of hemoglobin S, to evaluate the status and number of a person's red blood cells (RBCs) as well as hemoglobin level, and/or to determine whether a person has one or more altered hemoglobin gene copies. The presence of other abnormal hemoglobin variants may be seen but would require additional testing to identify specifically what type.
Prenatal testing
Doctors can diagnose sickle cell disease before a child is born (prenatally). Couples who are at risk for passing on this disease to their children can talk to their doctor about pre-natal test which includes:
-
Amniocentesis: the fluid surrounding the baby in the mother's womb (amniotic fluid) is extracted & sampled to look for the sickle cell gene. Testing before birth can be done as early as 8–10 weeks into the pregnancy
-
Chronic villus sampling
Infant screening
Sickle cell disease can be diagnosed at birth. Soon after birth, a sample of blood is taken from the infant's heel and sent to a lab, where it is screened for the presence of sickle cell hemoglobin (hemoglobin S).
Adult screening
If one member of a couple has sickle cell disease or sickle cell trait, the other member should be tested before becoming pregnant. This test requires a blood sample, which is screened for the presence of hemoglobin S, hemoglobin C, or beta-thalassemia.
Tests commonly performed to diagnose and monitor patients with sickle cell anemia include:
-
Bilirubin
-
Blood oxygen saturation
-
Complete blood count (CBC)
-
Hemoglobinopathy (Hb) evaluation: There are several methods of evaluating the type and relative amounts of various normal and abnormal hemoglobin types. These methods typically separate the different types of hemoglobin that are present so that they can be identified and quantified. They include:
-
Hemoglobin electrophoresis, traditionally used as the method to identify the presence of various hemoglobin’s
-
Hemoglobin fractionation by HPLC, the most frequently used method to screen for hemoglobin variants, including Hb S
-
-
Serum creatinine
-
Serum potassium
-
Sickle cell test
-
DNA Analysis: This test is used to investigate alterations and mutations in the genes that produce hemoglobin components. It may be performed to determine whether someone has one or two copies of the Hb S mutation or has two different mutations in hemoglobin genes (e.g., Hb S and Hb C).
-
Blood smear (also called peripheral smear and manual differential): The number and type of red blood cells are evaluated to see if they are normal. Sickle-shaped RBCs may be seen on the blood smear.
-
Iron studies: These may include: iron, ferritin, UIBC, TIBC, and transferrin saturation. These tests measure different aspects of the body's iron storage and usage. They are ordered to help determine whether someone has an iron deficiency anemia or an excess amount of iron (iron overload)
Sickle Cell Anemia Treatment
The goal of treatment is to manage and control symptoms, and to limit the number of crises. People with sickle cell disease need ongoing treatment, even when not having a crisis. It is best to get care from health care that take care of many patients with sickle cell anemia. People with this condition should take folic acid supplements. Folic acid helps make new red blood cells.
Treatment for a sickle cell crisis includes:
-
Blood transfusions (may also be given regularly to prevent stroke)
-
Pain medicines
-
Antibiotics
-
Pain relieving medicines
-
Hydroxyurea ( Droxia, hydrea)
-
-
Plenty of fluids
-
Supplemental oxygen: Breathing supplemental oxygen through a breathing mask adds oxygen to your blood and helps you breathe easier. It may be helpful if you have acute chest syndrome or a sickle cell crisis.
-
Treatment for children :
-
Routine childhood immunizations .
-
Daily antibiotics from 2 months to 5 years of age to prevent life-threatening infections. This practice stops at age 5 because older children don't have as many severe infections.
-
Multivitamin supplements with iron during infancy.
-
Folic acid supplements
-
Protein supplements if there is a lag in weight gain.
-
Starting at age 2 years, your child should get screened frequently with a transcranial ultrasound. This test measures blood flow in the arteries of the head and neck. If test results show a high chance for stroke, your child may get blood transfusions to lower the risk.
-
Prognosis
New and aggressive treatments for sickle cell disease are prolonging life and improving its quality. As recently as 1973, the average sickle cell anemia life expectancy for people with sickle cell disease was only 14 years. Currently, the life expectancy for these patients can reach 50 years and over.
The life expectancy of persons with sickle cell anemia is reduced. Some patients, however, can remain without symptoms for years, while others do not survive infancy or early childhood. Nevertheless, with optimal management, patients can now survive beyond the fourth decade.
Most patients suffer intermittent pain crises, fatigue, bacterial infections, and progressive tissue and organ damage. Impaired growth and development is the end result of the physical and emotional trauma that is endured by children with sickle cell anemia. Women with sickle cell live longer than their male counterparts. .